What Is a Laparoscopic Myomectomy?
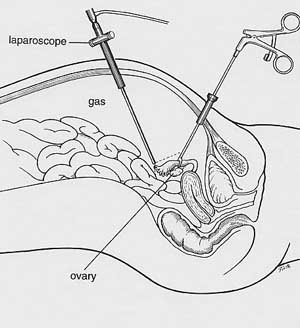
Laparoscopic surgery is usually performed as out-patient surgery under general anesthesia and has absolutely revolutionized gynecologic surgery because of the short hospital stay and quick recovery. The laparoscope is a slender telescope that is inserted through the navel to view the pelvic and abdominal organs. Two or three small, half-inch incisions are made below the pubic hairline and instruments are passed through these small incisions to perform the surgery. Because the incisions are smaller, patients can enjoy faster recovery times and smaller scars.
Laparoscopic surgery differs from traditional surgery in a few key ways: during laparoscopic surgery, the surgeon is not looking into the abdomen directly through a large incision across the abdomen, but performs the surgery while looking at a large video monitor suspended over the patient’s abdomen. The surgery, and especially the suturing of the uterus that is necessary during a laparoscopic myomectomy, requires a great deal of hand-eye coordination and dexterity, as well as knowledge of pelvic anatomy in order to be successful.
The procedure is very safe an effective when performed by a properly trained physician and the technique continues to evolve as new instruments are developed. However, many physicians today still lack the skills necessary to perform myomectomies through the laparoscope and therefore do not offer them to patients. Because of the small size of the incisions and the level of skill needed to correctly perform the surgery, this procedure is actually harder for a physician to perform without the proper experience and takes more skill and training than abdominal surgery.
I began performing operative laparoscopic procedures in 1987 and have been performing laparoscopic myomectomies for nearly 20 years. I have been teaching these techniques to other gynecologists since 1990 and am an internationally recognized expert in fibroid surgery and research. I am considered one of the best fibroid surgeons for laparoscopic or abdominal myomectomy in the United States and abroad and am able to perform laparoscopic myomectomy surgery with minimal blood loss, a short time under anesthesia for the patient, and with consistently good outcomes.
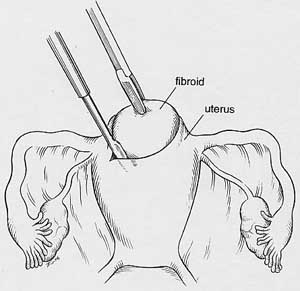
For laparoscopic myomectomy, a small scissors-like instrument is used to open the thin covering of the uterus. The fibroid is found underneath this covering, grasped, and freed from its attachments to the normal uterine muscle.
After the fibroid is removed from the uterus, it must be brought out of abdominal cavity. The fibroid is cut into small pieces with a special instrument called a morcellator, and the pieces are removed through one of the small incisions. New morcellators allow the easy removal of even large fibroids. The openings in the uterus are then sutured closed using specially designed laparoscopic suture holders and grasping instruments. Laparoscopic suturing with small instruments, in particular, requires special training and expertise. The entire procedure can take one to three hours, depending on the number, size, and position of the fibroids.
Myomectomy should be performed only if appropriate indications exist. And since it is a technically difficult surgery, your physician should have the extra training and experience that it requires. When talking to your doctor or interviewing a gynecologic surgeon, it is your right to ask about qualifications:
- How were you trained to do this surgery?
- How many of these operations have you performed for women with a situation like mine?
- Have you had any complications?
Many gynecologists have not been trained to suture with laparoscopic instruments, and some may even say that laparoscopic surgery is not possible. It is often a good idea to get a second opinion from a gynecologist who performs laparoscopic myomectomies on a regular basis to see if this procedure is feasible for you (see below).
Following laparoscopic myomectomy, most women are able to leave the hospital the same day as surgery. For more extensive surgery, a one-day stay may be a good idea. Because the incisions are small, recuperation is usually associated with minimal discomfort. Since the abdominal cavity is not opened to air, bacteria are less likely to reach the area of surgery, and the risk of infection is very low. The intestines are not exposed to the drying effect of air, or the irritating effects of the sterile gauze sponges used to hold the bowel out of the way during abdominal surgery. As a result, the intestines usually begin to work normally again immediately after laparoscopic surgery. This avoids the one- or two-day delay before a person is able to eat following regular abdominal surgery. After laparoscopic myomectomy, women usually can walk the day of surgery, drive in about 1 week and return to normal activity, work, and exercise within two weeks.
Video of a Laparoscopic Myomectomy
NEW! Watch in HD by clicking here
(graphic footage of actual surgery)
httpvh://www.youtube.com/watch?v=Fvw3dUesfdI
Can Laparoscopic Myomectomy be Performed if You Want to Have Children?
The use of laparoscopic myomectomy for women who desire to have children is controversial. The concern is how well the uterus will be able to withstand the stress of labor after having been cut and repaired with laparoscopic techniques. Fewer women have gone through labor and delivery after having a laparoscopic myomectomy than the numbers of women going on to have children after an abdominal myomectomy. The uterine scar, however, appears to heal as securely with a laparoscopic myomectomy as with myomectomy done by laparotomy. While many women have gotten pregnant and delivered safely, some physicians may recommend Caesarean section for delivery to avoid the stress of labor on the uterus. There are now a number of studies showing the safety and success of laparoscopic myomectomy for women who wish to get pregnant. However, a study comparing laparoscopic myomectomy and standard myomectomy with regard to fertility, labor, and delivery has not yet been performed by the research community. Further study will be needed to clarify this issue.
How Can We Remove a Big Fibroid Through a Small Laparoscopic Incision?
Less than a decade ago, removing fibroids after laparoscopic myomectomy was a difficult and time-consuming task. However, a few years ago an electrically powered device, called a morcellator, was invented and now allows us to quickly cut up the fibroid and easily remove it from the abdomen. The device is a hollow tube with a sharp circular blade at the end that rotates quickly and takes small slices off the fibroid in a few seconds. A large fibroid can now be removed in about fifteen minutes. Therefore, we are now able to perform laparoscopic myomectomy on women with even large fibroids. This device has allowed a major advance in our laparoscopic technique.
Which Fibroids Can Be Removed Laparoscopically?
The limits to laparoscopic myomectomy depend on a number of factors – the size(s), number and position of the fibroids, whether future fertility is desired, and the experience of the surgeon. Some of the issues are:
- How safe will the surgery be in terms of blood loss, time of anesthesia, and risk of injury to other organs,
- Strength of the repair of the uterus if fertility desired.
Size: Many experienced laparoscopic surgeons are comfortable removing fibroids less than 8 cm (3.5 inches) in diameter. Depending on the position of the fibroid, I have removed fibroids as large as 15 cm, and the largest reported in the literature is 16 cm.
Number: It is actually easier to remove 1 large fibroid than 10 small ones, because each fibroid may require a separate incision which then needs to be sutured. Suturing laparoscopically is more tedious than through an abdominal incision and is a skill that takes many years to perfect. Many experienced laparoscopic surgeons are comfortable removing up to 5 fibroids, but more may be reasonable in some situations.
Position: The easiest fibroids to remove are those that are outside the uterus on a stalk (subserosal pedunculated). Once the stalk is cut, the fibroid can be cut up into small pieces with a specially designed instrument called a morcellator and brought out of the abdomen through a small incision. The deeper the fibroid is into the uterine muscle wall, the more difficult it is to remove, and the more suturing needs to be done to repair the muscle wall. Other considerations regarding position include how close the fibroids are to the fallopian tubes (if fertility is desired) or to the uterine blood vessels, and whether there is any risk of damage to these areas. Skill, experience and judgment of the surgeon all come together here.
Fertility: If future fertility is desired, then the strength of the uterine wall repair is important. Therefore, the doctor must be able to suture the uterine wall with laparoscopic skill and care that is equivalent to the technique they would use for an abdominal surgery. If future fertility is not desired, then laparoscopic surgery can almost always be performed, again dependent on the sizes, number and position of the fibroids. MRI is a very helpful test that allows me to see the exact size, number and position of all the fibroids, so I always get an MRI before laparoscopic surgery. I like to show the MRI to the patient so that she can appreciate what the issues are and so we can discuss what is in her best interest.
These are the reasons why different gynecologists will give different opinions about whether laparoscopic myomectomy is feasible and appropriate – it is complicated. And, to a large degree, opinions will be based on the surgeon’s experience, skill and comfort doing laparoscopic myomectomy.
Can Myomectomy Lead to Scar Tissue?
Any surgery can cause scar tissue to form. Your body makes new tissue as part of the healing process to help connect things back together. This new tissue is called scar tissue or adhesions. Unfortunately, this natural defense can work against us when it occurs internally after surgery, because scar tissue may stick to and pull the normal tissue around it, sometimes causing pain. Scar tissue near the fallopian tubes or ovaries may decrease fertility by making it difficult for the egg to travel to the fallopian tube.
One of the major benefits of laparoscopic surgery is the principle that it causes fewer adhesions than abdominal surgery. A group of Italian doctors recently performed laparoscopy on a group of women a few months after they had fibroids removed by either laparoscopy or traditional abdominal surgery. The number of women studied was small (thirty-two), but the doctors found fewer and thinner adhesions in the women who had laparoscopic surgery. Further studies need to be performed, but this information is encouraging for women wishing laparoscopic surgery.
Can Adhesion Barriers Prevent Scar Tissue?
Another new advance in surgery has been the use of special substances, called adhesion barriers, which help prevent the formation of scar tissue after surgery. Small sheets of cloth-like material can be wrapped around the raw areas from surgery and the material prevents nearby tissue such as the intestines from sticking to the surgery sites. After a few weeks, the material dissolves, leaving the newly healed surgery sites fairly free of adhesions. While the barriers are not perfect, they have been shown to help reduce the formation of adhesions.
I am including an abstract of an article about one adhesion barrier, called Seprafilm:
Reduction of adhesions after uterine myomectomy by Seprafilm membrane (HAL-F): a blinded, prospective, randomized, multicenter clinical study. Seprafilm Adhesion Study Group.
Author: Diamond MP.
Fertil Steril. 1996 Dec;66(6):904-10.OBJECTIVE: To assess the safety and efficacy of Seprafilm (HAL-F), Bioresorbable Membrane, (Genzyme Corporation, Cambridge , MA ) in reducing the incidence, severity, extent, and area of uterine adhesions after myomectomy.
DESIGN: Prospective, randomized, blinded, multicenter study. Adhesion reduction was assessed by an independent, blinded, gynecologic surgeon who reviewed videotapes of each patient’s second-look laparoscopy.
SETTING: Nineteen institutions across the United States .
PATIENT(s): One hundred twenty-seven women undergoing uterine myomectomy with at least one posterior uterine incision > or = 1 cm in length.
INTERVENTION(s): Patients were randomized to treatment with Seprafilm or to no treatment at the completion of the myomectomy.
MAIN OUTCOME MEASURE(s): The incidence, severity, extent, and area of uterine adhesions at second-look laparoscopy.
RESULT(s): The incidence, measured as the mean number of sites adherent to the uterine surface, was significantly less in treated patients (4.98 +/- 0.52 [mean +/- SEM] sites) than in no treatment patients (7.88 +/- 0.48 sites) as were the mean uterine adhesion severity scores (1.94 +/- 0.14 versus 2.43 +/- 0.10; treatment versus no treatment, respectively), mean extent scores (1.23 +/- 0.12 versus 1.68 +/- 0.10), and mean area of adhesions (13.2 +/- 1.67 versus 18.7 +/- 1.66 cm2). No adverse events occurred that were judged to be related to the use of Seprafilm.
CONCLUSION(s): In this multicenter study, treatment of patients after myomectomy with Seprafilm significantly reduced the incidence, severity, extent, and area of postoperative uterine adhesions. Additionally, Seprafilm treatment was not associated with an increase in postoperative complications.
Should You Have a Robotic Myomectomy?
Both laparoscopic myomectomy and robotic myomectomy are considered minimally invasive surgery; they are performed through small (1/2 inch) incisions, and are outpatient procedures with a short recovery (about 14 days).During laparoscopic myomectomy the surgeon uses laparoscopic instruments to remove the fibroids and suture the uterus.The robotic uses similar instruments that are controlled by the surgeon sitting in a console a few feet away from the operating table (see photo).
After 15 years of experience performing and teaching laparoscopic myomectomies, I have now been trained and have started performing robotic myomectomies as well.To date, the only real benefit I see to using the robot is for women who wish to maintain their fertility and who have a fibroid that takes up the entire wall of the uterus.In these women, a slightly more precise suture repair of the wall may be (although not proven) beneficial to keep the wall strong during the later months of pregnancy.
In almost all other women, laparoscopic myomectomy is straight-forward and saves both time and money (the robot costs $1.5 million and requires $100,000 a year maintenance fee).Many gynecologists recently started using the robot because they have not been trained, or do not have the skill, to perform laparoscopic myomectomies and the robot does make suturing easier for them.So, up until now, these gynecologists were only able to offer their patients abdominal myomectomies.But, other than allowing the doctor to do an operation they could not do with laparoscopic instruments, there does not appear to be any benefit to the patient over laparoscopic myomectomy.
However, the recent infatuation with robotic surgery, both among doctors and women, as the “new thing on the block” concerns me.Unfortunately, gynecologists with little or no laparoscopic surgical expertise are using the robot as a marketing tool and using women as their guinea pigs.I recently heard about a few robotic surgeries that took 7 hours and the patients had scalp damage and hair loss from being tilted head-down on the operating table for so long.Another surgery took 5 hours, the surgeon left in smaller fibroids and the woman needed a blood transfusion.These situations seem irresponsible.
Women should be asking the same questions about robotics as they should be asking any surgeon – how many cases of robotic surgery have you done?How many for women with fibroids like mine?How long will this take?How many complications have you had and what were they?How many of your patients have required blood transfusions?Would this surgery be possible laparoscopically by someone with more experience?Would I be better served by someone else with more robotic experience?
As someone who teaches laparoscopic surgery to residents, fellows and other gynecologists on a regular basis, I fully understand the problem of doctors needing to get more experience and improve their skills.But, they should be starting with very easy cases and patient safety should be the primary (only) concern.Unfortunately, the robot company is pushing the robot very hard to gynecologists and hospitals, as well as marketing directly to women.Some of the cases described on message boards and elsewhere make it apparent that some physicians are getting in over their heads.So, make sure you are getting good care.
William H. Parker, MD
Clinical Professor, Reproductive Medicine, UC San Diego School of Medicine
Page last updated: January, 2018