What Is a Myomectomy?
Myomectomy means the surgical removal of just the fibroid, with reconstruction and repair of the uterus. There are now a number of techniques used to perform myomectomy: through an abdominal incision, vaginal incision, with a laparoscope, or with a hysteroscope. Myomectomy relieves symptoms in more than 75% of women. “The restoration and maintenance of physiologic (normal) function is, or should be, the ultimate goal of surgical treatment”, said Victor Bonney, an early advocate of abdominal myomectomy, in 1931. However, women are often told that myomectomy is not appropriate for them because hysterectomy is safer, is associated with less bleeding or that uterine muscle cancer (sarcoma) may be present. However, recent studies dispute all of those claims.
Studies show there may actually be less risk of complications during myomectomy than during hysterectomy. One study of women who had myomectomies and women who had hysterectomies for fibroids of the same sizes (about 4 months pregnancy size) found surgery took slightly longer in the myomectomy group (200 v. 175 min), but there was more blood loss in the hysterectomy group. The risks of bleeding, fever, life-threatening complications, need for another surgical procedure or re-admission to the hospital were not different. The authors of the study concluded that there was no difference in complications and with an experienced surgeon myomectomy is a safe alternative to hysterectomy.
More about surgery and recovery can also be found at A Gynecologist’s Second Opinion: http://www.gynsecondopinion.com/surgery.htm
What Is an Abdominal Myomectomy?
The most common method of removing fibroids is by making a four- to six-inch “bikini” incision on the abdomen just below the pubic hairline.
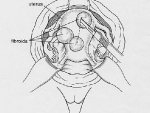
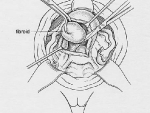
After inspecting the uterus to determine the number and position of the fibroids, the uterus is injected with pitressin, a solution that limits bleeding during the surgery. Then the covering of the uterus overlying the fibroid is cut (illustration 1), and the fibroids are separated and removed from the normal uterine muscle (illustration 2). In that fibroids push away normal uterine muscle as they grow (and do not destroy it), the normal uterine muscle can be sewn back together (illustration 3). This procedure takes about one to two hours, depending on the number, sizes and positions of the fibroids. Following surgery, a woman having an abdominal myomectomy may need to stay in the hospital for two to three days.
For information about recovery (and other issues) from women with fibroids, see:
http://health.groups.yahoo.com/group/uterinefibroids/
Can Adhesion Barriers Prevent Scar Tissue?
Another new advance in surgery has been the use of special substances, called adhesion barriers, which help prevent the formation of scar tissue after surgery. For abdominal myomectomy, small sheets of thin transparent material can be wrapped around the raw areas from surgery and the material prevents nearby tissue such as the intestines from sticking to the surgery sites. After a few weeks, the material dissolves, leaving the newly healed surgery sites fairly free of adhesions. While the barriers are not perfect, they have been shown to help reduce the formation of adhesions.

The adhesion barrier Seprafilm is teased out of its paper protection onto the incision in the uterus. The Seprafilm will dissolve within 2 weeks, after the uterine incision has started to heal.
New Pain Management Techniques Used Following Surgery
The first few days after surgery are the hardest, and research is always being done in an effort to ease postoperative discomfort. I use an innovative device to relive post-operative pain called “ON-Q”. As we are finishing surgery two tiny plastic tubes are inserted underneath the incision. The tubes are connected to a tennis ball sized device that slowly and evenly pushes local anesthetic contained in the ball into the incision – exactly where you need it. The device is used for 3 days and then easily, and absolutely painlessly, removed. This device greatly reduces the need for injected pain medication which travels throughout the entire body and brain and causes the grogginess that often accompanies narcotics.
I also commonly prescribe another effective innovation called “Patient Controlled Analgesia” (PCA). With this method, a small bedside pump drips pain medication into your IV at a very controlled, slow, and steady rate. With this steady low level of medication, you should not develop significant pain and the total amount of medication necessary per day is much smaller than with shots. Therefore, you will not feel as groggy, and the pain relief is much better.
The catheter has small holes that allow the local anesthetic to be sprinkled under the incision area.
Are Some Fibroids Too Big for an Abdominal Myomectomy?
The short answer is NO. Some doctors and some managed-care organizations have policies stating that an abdominal myomectomy cannot be attempted if the uterus is bigger than a certain size (usually a three-month pregnancy size). Hysterectomy is the only option that they will offer. However, gynecologists who are skilled and experienced at myomectomy surgery can perform an abdominal myomectomy on just about any size uterus (see photo gallery below). One of the risks of a myomectomy is bleeding from the uterus during surgery. However, there are a number of techniques that can be used to reduce bleeding. A medication can be injected into the uterus that causes the blood vessels in the muscle to constrict, and less blood will seep out of the incisions in the uterine wall. Or the doctor can place an elastic tourniquet around the lower portion of the uterus to decrease the blood flow to the uterus.
Abdominal Myomectomy video – 20 week size uterus. Video is graphic
httpvh://www.youtube.com/watch?v=QMKJ9IoTdD0
The placement and depth of the incisions on the uterus are also important. Making the incisions down to the area between the fibroid and normal muscle, where there are very few blood vessels, will reduce bleeding. Closing every incision quickly and tightly will promptly stop bleeding.
A cell saver is a surgical machine that suctions blood from the surgery site, washes it with sterile salt water, filters it and then gives the patient their own blood through her IV. Therefore, there is less need to give your own blood before surgery and less need for a blood transfusion, avoiding the risk of infection or transfusion reaction. Although I rarely need to use the cell-saver, I have it available outside the room for every myomectomy surgery. If needed, it takes only a few minutes to set up. For women who have very numerous, large fibroids, I set the cell-saver up right at the beginning of the surgery. If I need it, it is ready to go.
In a study of 91 women with fibroids larger than 16 weeks (ranging from 16 to 36 weeks), no one needed to have the surgery changed to a hysterectomy. Complications were very rare and, by using a cell-saver, very few women (7) required a blood transfusion. Many gynecologic surgeons don’t have training in these techniques and so don’t offer them. Dr. Parker is considered one of the best fibroid surgeons for abdominal or laparoscopic myomectomy in the United States and abroad and is able to perform myomectomy surgery with minimal blood loss, a short time under anesthesia for the patient, and with consistently good outcomes. He is also an internationally recognized expert in fibroid surgery and research. Ask your doctor and get some clarification on their experience with myomectomy surgery.
Avoiding the Need for Blood Transfusion
Donated blood, even if you donate your own blood, decreases in quality every day it sits in the blood bank. The blood cells become more fragile and when they are transfused they clog up capillaries and block blood flow and oxygen delivery to the body’s cells.
Studies show that ill patients in an ICU who were transfused had more problems than patients with similar levels of anemia who did not get transfused. Although serious problems are less of a risk for young, healthy women who are having myomectomies (compared to 80 year-olds in an ICU!), the best strategy is for you to get your blood count up before surgery and the use of a cell-saver during surgery.
If your blood count is very low (hemoglobin levels below 9), I usually use Procrit to stimulate red blood cell production for about 3 weeks before surgery. This medication is exactly like the protein made by the kidney that tells the bone marrow to make more red blood cells. It is important to also take high doses of iron to provide your body with the building blocks to make red blood cells. Vitamin C (1000 mg/day) should also taken, which helps you absorb more iron through the intestines. There is no magic number, but it is safer to have the hemoglobin 10 or higher before surgery. In some women, very heavy menstrual bleeding does not allow us to get the blood counts up even with Procrit and Vitamin C (very rare), but this usually works well.
A number of surgical techniques can be used to reduce the risk of blood loss during surgery. I use Pitressin, a medication that makes blood vessels constrict and which has been shown to effectively decrease blood loss during myomectomy. It is important to find the exact area where the fibroid starts and the normal uterine muscle ends – this is the area where the fewest blood vessels are found and where the least amount of bleeding occurs when removing the fibroid. After each fibroid is removed, it is important to suture closed the hole in the normal uterine muscle so that bleeding is stopped immediately.
An additional strategy is the use of the cell saver, which allows me to replace blood loss, if necessary, immediately during surgery with the patient’s own fresh blood before the blood has a chance to deteriorate. In addition, with the cell-saver, since you get your own blood there is no risk of HIV, hepatitis or mismatched blood.

Blood is suctioned from the incision and operative area, stored in the canister, and then filtered and returned to the patient through an IV
And lastly, the current recommendation is to not get a blood transfusion unless it is really necessary: if you are very dizzy or weak when you stand up, or if your hemoglobin is below 7 (normal is 12). Since the transfused blood doesn’t work very well, it is better and safer to take lots of iron and let your body to build up your own blood count slowly during the recovery period.
What are the risks of abdominal myomectomy?
Some studies suggest that there may be less risk of intraoperative injury with abdominal myomectomy compared to abdominal hysterectomy. One study of women having surgery for fibroids showed that operating times were slightly longer in the myomectomy group, but blood loss was slightly more in women who had a hysterectomy. The risks of severe complications such as severe bleeding, fever, life-threatening problems or need for readmission to the hospital were the same for both groups of women. However, 13% of women in the abdominal hysterectomy group had a complication, including 1 bladder injury, 1 ureteral injury, 3 bowel injuries, 8 women who had nausea, vomiting and slow return of bowel movements, and 6 women with pelvic infections. In contrast, complications occurred in only 5% of the abdominal myomectomy patients, including 1 bladder injury, 2 women who needed another operation for a bowel obstruction and 6 women who had nausea, vomiting and slow return of bowel movements. The authors concluded that myomectomy should be considered a safe alternative to hysterectomy.
What Does the Incision for an Abdominal Myomectomy Look Like?
I am often asked what the incision will look like after an abdominal myomectomy. I always make a bikini incision (medical name is Pfannensteil incision after the doctor who developed it). The incision is about 1 inch above the pubic bone and 4-6 inches long, depending on the size of the fibroids. The tissue underneath the skin called the fascia is then cut to allow access to the abdominal cavity. I do not cut the muscles, but stretch them apart (they have a natural separation) in order to get to the uterus and fibroids. The incision heals nicely as can be seen in the photos.
Can a Myomectomy Be Performed During a Cesarean Section?
Experienced surgeons can safely perform a myomectomy in carefully chosen women during a Cesarean section. One study of twenty-five women who had myomectomies performed for fibroids between 2 and 10 cm, showed that although five women needed a blood transfusion, no one needed to have a hysterectomy. Another study found that less than 1% of women needed a transfusion and none required hysterectomy. The authors concluded that, in experienced hands, myomectomy may be safely performed in some women during Cesarean section.
William H. Parker, MD
Clinical Professor, Reproductive Medicine, UC San Diego School of Medicine
Page last updated: January, 2018