What Is Uterine Fibroid Embolization?
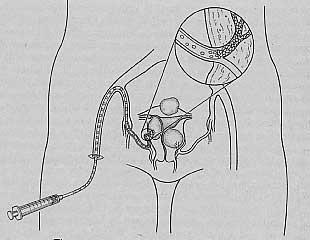
Uterine fibroid embolization (UFE) is a non-surgical technique that shrinks fibroids without removing them. The procedure is performed by an interventional radiologist, an M.D. with basic certification in radiology and special education and certification in interventional radiology. You do not need to be put to sleep, but sedating medications are given in the vein to help you relax during the one to two hours the procedure takes. A small (one-inch) incision is made in the groin directly over the artery carrying blood to the leg. The interventional radiologist guides a long thin catheter (tube) into the blood vessels that supply the uterus while monitoring the process under X-ray. Small plastic particles are pushed through the catheter until they form a blockade to the blood flowing to the uterus. Fibroids have a limited supply of blood vessels, and with the blood flow blocked, the fibroid cells start to die off. The surrounding normal uterine muscle has a better blood supply and is able to survive. Deprived of blood, nutrition, and oxygen, fibroids shrink like prunes for the three to six months following embolization, and the symptoms from the fibroids often lessen as well.
It has now been performed in about 30,000 women in the United States and another 20,000 women worldwide.
What Is Recovery Like After UFE?
After embolization blocks the blood supply to the fibroids, the cells of the fibroid start to die off immediately. The dying cells release toxins that irritate the surrounding tissue and cause pain and inflammation. Almost all women have moderate to severe pain for the first day or so after uterine artery embolization and are kept in the hospital for one day so that they can be given narcotic pain medication. Anti-inflammatory medications, like Anaprox or ibuprofen, are also given to keep the inflammation down in the uterus. Tylenol is given for the fever that commonly follows the procedure.
However, most women are able to go home the next morning and only need to take oral pain and anti-inflammatory medications for the next few days. As with all medical procedures, the recovery varies from woman to woman. Many women feel back to normal within a few days and return to regular activity within a week or so. Other women have pain or discomfort for weeks and may not get back to normal activity for a few weeks or, rarely, even months.
How Effective and Safe Is UFE?
Many women will notice a relief of fibroid symptoms within six weeks after the procedure. However, it takes a few months for the fibroids to fully shrink and the full effect of the procedure to be evident. Three to six months following UFE, the uterus and fibroids will have decreased about 40 percent in size. About 90 percent of women who were bothered by symptoms related to the size of their fibroids will have a significant improvement and be satisfied with the results. Likewise, about 85 percent of women who had heavy bleeding from their fibroids will have lighter and shorter periods and be satisfied with the results. About 10 to 15 percent of women who have UFE will continue to have bothersome symptoms and usually require other treatment. Many of the initial women who had UFE have now been followed for three years and are still symptom free. Because the procedure has only been widely available since 1997, we do not have longer follow-up on these women yet.
About 25,000 women worldwide have had UFE performed for uterine fibroids. To date, the procedure has been extremely safe. The Society of Interventional Radiology reports only four deaths from this procedure or 1 out of every 6,000 women who have had UFE. For comparison, the risk of dying from surgery or anesthesia for a hysterectomy is about 2 out of 6,000 women. Risks for an individual are related to your medical condition, your age, and the disease for which you are being treated. Comparing risks of UFE to hysterectomy for women of similar age and condition with fibroids, it appears that the serious risks may be slightly lower with UFE.
I am including an abstract of a recent and large UAE study:
The Ontario Uterine Fibroid Embolization Trial. Part 2. Uterine fibroid reduction and symptom relief after uterine artery embolization for fibroids.
Authors: Pron G, Bennett J, Common A, Wall J, Asch M, Sniderman K; Ontario Uterine Fibroid Embolization Collaboration Group.
Fertil Steril. 2003 Jan;79(1):120-7.
OBJECTIVE: To evaluate fibroid uterine volume reduction, symptom relief, and patient satisfaction with uterine artery embolization (UAE) for symptomatic fibroids.
DESIGN: Multicenter, prospective, single-arm clinical treatment trial.
SETTING: Eight Ontario university and community hospitals.Five hundred thirty-eight patients undergoing bilateral UAE.
INTERVENTION(S): Bilateral UAE performed with polyvinyl alcohol particles sized 355-500 microm.
MAIN OUTCOME MEASURE(S): Three-month follow-up evaluations including fibroid uterine volume reductions, patient reported symptom improvement (7-point scale), symptom life-impact (10-point scale) reduction, and treatment satisfaction (6-point scale).
RESULT(S): Median uterine and dominant fibroid volume reductions were 35% and 42%, respectively. Significant improvements were reported for menorrhagia (83%), dysmenorrhea (77%), and urinary frequency/urgency (86%). Mean menstrual duration was significantly reduced after UAE (7.6 to 5.4 days). Improvements in menorrhagia were unrelated to pre-UAE uterine size or post-UAE uterine volume reduction. Amenorrhea occurring after the procedure was highly age dependent, ranging from 3% (1%-7%) in women under age 40 to 41% (26%-58%) in women age 50 or older. Median fibroid life-impact scores were significantly reduced after UAE (8.0 to 3.0). The majority (91%) expressed satisfaction with UAE treatment.
CONCLUSION(S): UAE reduced fibroid uterine volume and provided significant relief of menorrhagia that was unrelated to initial fibroid uterine size or volume reduction. Patient satisfaction with short-term UAE treatment outcomes was high.
Are You a Good Candidate for Embolization?
Embolization is still a relatively new procedure, and selecting the appropriate women who will clearly benefit from UFE is still a work in progress. There remains some difference of opinion among interventional radiologists, and even more differences between gynecologists and interventional radiologists, as to which women should have the procedure. If shrinking the fibroids to a little more than half their present size would relieve your symptoms, then UFE may be right for you.
However, UFE may not be very helpful for women with extremely large fibroids because they may not shrink enough to make a significant difference in the symptoms. Women with fibroids on a stalk outside the uterus, called pedunculated fibroids, should not have UFE. Embolization can cause the stalk to deteriorate and allow the fibroid to float around the abdominal cavity. The dead tissue causes an inflammation inside the abdomen resulting in pain and fever. Surgery may be required to remove the degenerating fibroid. Fibroids that mostly bulge inside the uterine cavity, submucus fibroids, may also detach and float inside the uterine cavity after embolization. The uterus will then cramp and contract to expel the fibroid. Discharge and blood may accompany this process, and sometimes infection develops. If the fibroid is not expelled, surgery may be needed to remove it.
What Is Post-embolization Syndrome?
Following UFE, some women may develop fever, increasing rather than decreasing pelvic pain, and a vaginal discharge. This combination of symptoms is called post-embolization syndrome. Many of these women will also experience nausea and exhaustion. The symptoms may last for days or even weeks and cause concern because of the possibility that serious infection is present in the uterus. If the symptoms get worse over time, rather than better as would be expected, then an examination and evaluation for infection is important. Post-embolization syndrome will resolve over time, even if it takes a few weeks. However, if infection is present in the uterus, hysterectomy is usually necessary to prevent the spread of a very serious infection throughout the body. This infection, called sepsis, has led to the deaths of 2 women (out of 25,000) following UFE. Good communication between the gynecologist and interventional radiologist will be helpful to differentiate between post-embolization syndrome and infection.
What Are the Long-Term Risks of UFE?
Uterine fibroid embolization was first performed to shrink fibroids in 1995 and has only been widely available since 1997. For that reason, there is presently no long-term follow-up information. However, since embolization has been used for a long time for other reasons, we do know that it is very safe. There have not been any allergic reactions to the particles. Also, there is no evidence, or even any reason to believe, that embolization could cause cancer of the uterus.
Some women worry that the particles will travel to other parts of the body during the procedure or at a later time. Misembolization, particles traveling during the procedure, is discussed below. After the procedure, the particles become embedded into the vessel wall by scar tissue and do not travel in the bloodstream. After about six weeks, the blood vessels open back up and start supplying blood to the uterus again. Since the fibroids have already died off, they do not grow back again.
Childbirth after embolization is now viewed with caution. We know that women who have had embolization of the uterus for hemorrhage following childbirth have been able to safely have more children. However, those women have not had embolization for fibroids, a somewhat different situation. Fibroids are an integral part of the uterine wall, and embolization destroys them. Therefore, the strength of the remaining tissue is uncertain. Hopefully, further study will clarify whether childbirth is safe after UFE.
Complication Rates and Effectiveness of Uterine Artery Embolization
Title: Complication Rates and Effectiveness of Uterine Artery Embolization in the Treatment of Symptomatic Leiomyomas: A Systematic Review and Meta-Analysis
Journal: American Journal of Roentgenology, 2012; volume 199, pages 1153-1163.
Authors: Sundeep S. Toor, Arash Jaberi, D. Blair Macdonald, Mathew D. F. McInnes, Mark E. Schweitzer and Pasteur Rasuli.
Study from: Department of Medical Imaging, Ottawa Hospital, Ontario, Canada.
Problem: Many studies of uterine artery embolization include small numbers of women and conclusions are difficult to make. A “meta-analysis” combines the results of many studies and analyzes them together in order to improve the accuracy of the conclusions.
Study: The study determined the rates of complications, need for other treatment after UAE and the rate of success of uterine artery embolization (UAE) for the treatment of fibroids.
Results: Fifty-four published studies were analyzed including 8,159 patients. Women were followed anywhere from 3 months to 5 years after UAE in the various studies. There were no reported deaths in these studies. Major complications occurred in 3% of women, including serious infection in 2%. About 1% of women needed a hysterectomy to treat complications of UAE. Four percent of women had permanent loss of menstrual periods. Every year after UAE, 5% of women needed either a repeat UAE, a myomectomy or a hysterectomy due to failure of UAE to help symptoms. Most of the failures occurred in the first 2 years after UAE. About 3% of women needed to be readmitted to the hospital. Other complications included passing fibroid tissue through the vagina after UAE (5%). Fewer complications occurred in recent studies than in the early studies of UAE as techniques have improved. UAE was successful for 78% to 90% of women.
Authors’ Conclusions: UAE is an effective procedure for treatment of symptomatic uterine fibroids with a low rate of major complications, supporting its use as an alternative to hysterectomy.
Dr. Parker’s Comments: The results of this study of more than 8,000 women who had UAE are very reassuring. 80-90% of women are satisfied with UAE. Also, the risk of having a major complication from UAE is lower than for hysterectomy. However, the need for readmission to the hospital after UAE or the need for another fibroid treatment is greater than the rates for hysterectomy.
What Is Misembolization?
The particles that are used for embolization are very small, about the size of a grain of sand. In a few instances, the particles have been noted to travel through blood vessels to areas other than where they were intended to go. We call particles ending up in the wrong place non-target embolization, or misembolization. We do not know how often this happens, but it appears to be uncommon.
In an attempt to avoid these complications, many interventional radiologists are paying close attention to the pattern of the blood vessels in the pelvis for every patient, noting that the path of the vessels can be different from woman to woman. An attempt is made to avoid vessels going anywhere other than the uterus. However, the vessels supplying one area may interconnect with the vessels of another area. If this is the case, it may be difficult to completely avoid particles going to other areas. In over 25,000 women having UFE to date, serious misembolization has only been reported in a very few.
Can UFE Affect Fertility?
The answer is maybe. Misembolization, or particles travelling to unintended areas as described above, may rarely block off blood flow to the ovaries and interfere with the function of the ovaries. In addition, in about 10 percent of women, the main blood vessels supplying the ovaries start as a branch from the uterine artery. If the uterine artery is blocked, the blood supply to the ovaries is also blocked, and the ovaries cease functioning. Following embolization, in about 5 percent of women, the ovaries stop functioning, and early menopause follows. While this is never a good thing at any age, it is devastating for a twenty-five-year-old woman who wishes to have children.
Another unanswered question is whether the age of menopause will be affected in women who have UFE. If misembolization allows particles to block blood flow to some eggs, those eggs may die. The ovaries have many eggs, and the surviving eggs may continue to produce some hormone even if lots of other eggs have been destroyed. Hormone tests during this time may appear normal. However, if fewer eggs than normal remain in the ovaries, both eggs and the hormones they produce may be depleted before normal menopause is expected, around age fifty-two. We do not know whether any women who have had UFEs are destined to enter earlier menopause. This question will take many years to answer.
The problem of early menopause has been seen after hysterectomy in some women. If the blood vessels supplying the uterus also have a branch as the main supply to the ovaries, then suturing the uterine arteries during the hysterectomy will destroy the ovaries. Myomectomy, which does not disturb the uterine or ovarian blood vessels, has not been found to cause this problem.
Pregnancies and healthy babies have been born to women who have had UFE. However, we do not know how many women tried to get pregnant and were unsuccessful. We do not know how many had a miscarriage. To date, no cases of rupture of the uterus during pregnancy or labor have been reported following UFE. However, since the number of women getting pregnant after UFE is very small, we do not know what the risk really is. As a result of all this uncertainty, most interventional radiologists recommend that women who wish to have children not use UFE as treatment for their fibroids.
Are There Surgical Techniques That Mimic UFE?
There has been a bit of discord between some gynecologists and interventional radiologists over UFE as treatment for fibroids. Some of this disagreement is medical-an honest debate about which women will benefit most from UFE instead of myomectomy or hysterectomy-and some of the disagreement is self-interest and economics. Gynecologists recently created a surgical technique to tie off the uterine arteries (rather than block them with particles) using the laparoscope. So far, the first two years of results in a small number of women have been as good as those achieved with UFE. There may be advantages to the surgical approach, called laparoscopic uterine artery ligation, and there are some clear disadvantages. The current surgical approach requires an anesthetic and is an invasive procedure with the risks of any laparoscopy. However, the surgical approach only ties off the uterine artery, and since no particles are used, there is no risk of misembolization to other areas.
Laparoscopic uterine artery ligation may, theoretically, decrease the small risk of premature menopause that accompanies UFE. If, however, some women have a branch of the uterine artery as the only blood supply to the ovaries, then surgical ligation of the uterine artery will cut off blood supply to the ovaries, and the result will be early menopause for these women. A variation of this surgical technique that is being developed blocks the uterine artery though a small vaginal incision and does not require general anesthesia, and thus avoids some risk. It is still too early to tell whether there will be any long-term differences between these techniques, so you will need to ask your doctor about new results as they are published.
How Do You Find a Doctor to Perform UFE?
Interventional radiologists, M.D. sub-specialists in the field of radiology, perform uterine artery embolization. Interventional radiologists are not only trained to interpret X-rays, but they take three years of special training and are certified to place catheters into blood vessels to deliver medications or, in these cases, particles to block blood flow. As is true for gynecologists and gynecologic surgery, some interventional radiologists have more experience with UFE than others. You need to ask the same questions you would ask of your surgeon: How many of these procedures have you performed? How many in cases similar to mine? How many complications have you had, and what was the extent of those complications?
The other important issue to consider is whether UFE is right for you in the first place. Unfortunately, interventional radiologists are not trained in gynecology, and there may be other less invasive treatments available to treat your symptoms. It might be best to get a second opinion from a gynecologist in addition to an opinion from an interventional radiologist before choosing treatment. UFE has been performed on women who were not appropriate candidates for the procedure and who would have been better off with another type of treatment. Hopefully, in the future, more gynecologists and interventional radiologists will work together to help guide women to treatment options that are right for them without regard to monetary gain or other self-interests.
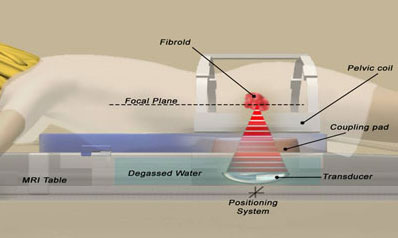
Can Focused Ultrasound (MRgFUS) be Used to Treat Fibroids?
Ultrasound uses high-frequency energy in the form of sound waves. This energy can be focused on a single point inside a woman’s body (for instance on a fibroid) so that the heat created by the energy destroys fibroid cells. This is like focusing a lens to burn a hole in a leaf. And just as you can pass your hand above the leaf without feeling any heat because the energy is not focused there, the ultrasound energy can pass through the body without harming it until it gets to the focal point in the fibroid. MRI is used to focus the ultrasound waves, hence the term MRgFUS (Magnetic Resonance guided Focused Ultrasound).
Still in early development, focused ultrasound is a non-invasive alternative to treat some women with fibroids. The advantages of focused-ultrasound are very low risk and very rapid recovery, with return to normal activity in one day. Presently, the procedure is not recommended for women wishing future fertility because no women have become pregnant after the procedure and the safety of pregnancy after MRgFUS is not known.
In published studies, the FDA limited the area treated to about 10% of the fibroid size, and women had only a 15% reduction in fibroid size 6 months after treatment. Two years after treatment there was only a 4% reduction in fibroid size. Six months after treatment 71% of women had fewer symptoms, but at the end of a year only about 50% still had less bothersome symptoms and 23 of 82 women (28%) had chosen to have a hysterectomy, myomectomy or UAE. One woman had an injury to her sciatic nerve due to ultrasound energy and 5% of the women had minor skin burns. Once the FDA allows larger areas to be treated, we would expect to see greater success, but we will also need to see whether there will be increased risks. Hopefully, as the technology improves, MRgFUS will be another proven alternative for women with symptomatic fibroids.
William H. Parker, MD
Clinical Professor, Reproductive Medicine, UC San Diego School of Medicine
Page last updated: January, 2018