About Hysterectomy
While bothersome symptoms such as very heavy bleeding or pain often respond to medications or other non-surgical treatment, sometimes the symptoms do not get better. For some women, other minimally invasive surgical techniques may have failed hysterectomy may be appropriate. A recent American study done by a woman doctor at Harvard found that many women who had a hysterectomy performed because of moderate or severe symptoms were “very satisfied” with the results of surgery, and they noted an improvement in their quality of life.
One of the most important factors in helping you choose appropriate medical care is your full understanding of the reasons for treatment, the risks, and the potential benefits for you. If hysterectomy has been suggested to you as an option, you should carefully weigh the potential benefits and risks so that you are able to make a comfortable and informed decision about whether hysterectomy is right for you. Hopefully, the information presented here will help you with this decision.
Myomectomy as a Surgical Alternative to Hysterectomy
“The restoration and maintenance of physiologic (normal) function is, or should be, the ultimate goal of surgical treatment”, said Victor Bonney, an early advocate of abdominal myomectomy, in 1931. Myomectomy means the surgical removal of just the fibroid, with reconstruction and repair of the uterus. However, women are often told that myomectomy is not appropriate for them because hysterectomy is safer, is associated with less bleeding or that uterine muscle cancer (sarcoma) may be present. Recent studies dispute all of those claims.
There may actually be less risk of complications during myomectomy than during hysterectomy. One study of women who had myomectomies and women who had hysterectomies for fibroids of the same sizes (about 4 months pregnancy size) found surgery took slightly longer in the myomectomy group (additional 25 min), but there was more blood loss in the hysterectomy group. The risks of fever, life-threatening complications, need for another surgical procedure or re-admission to the hospital were not any higher for the women having a myomectomy. The authors of the study concluded that with an experienced surgeon myomectomy is a safe alternative to hysterectomy.
There are two main types of myomectomy: laparoscopic myomectomy and abdominal myomectomy.
What Are the Different Types of Hysterectomy?
Hysterectomy, removal of the uterus, can be performed through an abdominal incision, an incision at the top of the vagina, or laparoscopically through a few small (1/2 inch) incisions in the abdomen.

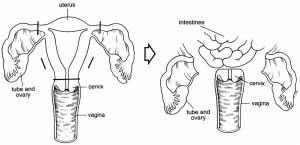
Total hysterectomy removes the entire uterus, including the cervix. (Click on image to open a larger version in a new window)
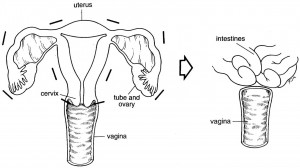
Removal of the ovaries and tubes, which is rarely a good idea, is called bilateral salpingo-oophorectomy. (Click on image to open a larger version in a new window)
Supra-cervical hysterectomy removes only the upper body of the uterus and the cervix is left in place, attached to the top of the vagina. Unless you have cancer or have had recurrent problems with pre-cancer of the cervix you can have a choice as to whether the cervix will be removed or not. Some women feel that if the cervix is removed they will have diminished sexual pleasure or will develop bladder problems. This issue is discussed in detail below.
For patients who have known or suspected pelvic scar tissue or endometriosis, laparoscopic surgery allows the surgeon to remove the diseased tissue with the laparoscope before performing the hysterectomy. For patients who have large fibroids that might otherwise be difficult to remove by vaginal hysterectomy, laparoscopic hysterectomy allows the surgeon to detach the blood vessels to the uterus while viewing them through the laparoscope and skilled laparoscopic surgeons can remove even very large fibroid uteri laparoscopically and thus avoid a large abdominal incision. Laparoscopic hysterectomy does require extra training and considerable skill and experience on the part of the surgeon.
Laparoscopic hysterectomy and laparoscopic subtotal hysterectomy will be described here. Abdominal and vaginal hysterectomies are more fully discussed at: http://www.gynsecondopinion.com/.
Laparoscopic Hysterectomy
Laparoscopic hysterectomy, either total or supracervical, is often possible for women with fibroids, with the benefits of less postoperative pain, shorter hospital stay and faster recover
Laparoscopic Supracervical Hysterectomy
We pride ourselves in performing hysterectomies usually as a last resort to gynecologic problems, but the operation is sometimes necessary and appropriate. Dr. Parker has a superb reputation for gynecologic surgery in general and laparoscopic surgery specifically. He has been performing operative laparoscopic surgery since 1987 and laparoscopic hysterectomies since 1993.
One advantage of laparoscopic hysterectomy is that the incisions are smaller (1/2 inch) and much less uncomfortable than that of abdominal hysterectomy. Also, the hospital stay of 0-1 day and the ability to resume normal activity in about 2 weeks are substantially shorter than for abdominal hysterectomy (3 days in the hospital and 6 weeks recovery) and slightly shorter than for vaginal hysterectomy (1-2 days, 3-4 weeks).
Laparoscopic supracervical hysterectomy allows the uterus to be detached from inside the body using laparoscopic instruments while the doctor is viewing the uterus, tubes, and ovaries on a flat screen monitor using a camera attached to a telescope. This procedure differs from standard hysterectomies in that the cervix is retained in the woman’s body, while the main portion of the uterus is detached and removed through small (one inch) incisions in the lower abdomen. One of the instruments making this surgery feasible is called an electronic morcellator, which cuts the uterus into small pieces so that the tissue can be removed through the small incisions.
Is There Any Benefit to Leaving the Cervix in Place?
There is much debate as to whether there is any benefit to not removing the cervix. The proponents of supracervical hysterectomy suggest that bladder and sexual function are better preserved with this operation. These potential benefits have not been borne out by statistical analysis of two recent large studies, but some women may still note changes in sexual satisfaction, or bowel or bladder function if their cervix is removed and may benefit from keeping it. So, this is something you should think about and ask your doctor about. Also, it does appear that healing and recovery are somewhat faster because there is no surgery performed inside the vagina and no stitches at the top of vagina that need to heal. Since the cervix is still in place after supracervical hysterectomy, it is important to continue to have Pap smears regularly.
Dr. Parker has extensive experience performing both laparoscopic supracervical hysterectomies and total laparoscopic hysterectomies for many years and his patients’ experience has been extremely favorable. There are indications and reasons for each procedure, and before surgery he discusses these issues with each patient who is considering a hysterectomy.
httpv://www.youtube.com/watch?v=J9Q1g2RTNLA
What Is a Total Laparoscopic Hysterectomy?
Total laparoscopic hysterectomy is a surgical procedure that allows both the uterus and cervix to be detached from inside the body by laparoscopic instruments and then they are removed through a small incision at the top of the vagina. For women who have cervical conditions that require removal of the cervix (persistent abnormal pap smears, etc), this procedure allows removal of the cervix.
Will Hysterectomy Become a Less Common Operation?
New treatments for fibroids and abnormal bleeding, two of the most common reasons for hysterectomy, should decrease the need for hysterectomy. Myomectomy performed by hysteroscopy, laparoscopy, or abdominal surgery can usually be used to remove fibroids and alleviate symptoms without needing to remove the uterus.
Abnormal bleeding may often be treated by the progesterone IUD OR endometrial ablation with 90% of women reporting excellent results, which allows these women to avoid hysterectomy. Endometriosis, the third most common reason for hysterectomy, may be treated by medical therapy although the side-effects and expense of the medications limit its use. However, laparoscopic surgery to remove just the areas of endometriosis may also be used to alleviate pelvic pain associated with endometriosis. Hysterectomy, for most of these conditions, should be a last resort, not the first one.
What Questions Should You Ask Your Doctor if it is Recommended that you have a Hysterectomy?
It is important for you to understand the reasons that your doctor has suggested a hysterectomy as treatment for your gynecologic problem. The most common reasons for surgery are pain, bleeding, or symptoms from fibroids. The first question that you should ask is what is specifically causing your problem. You should also ask if there are other tests that can be done to make the diagnosis more certain.
Once a probable diagnosis has been established, you should also ask what the consequences to your health will be if you do not have surgery, either at all, or at this time. For every condition, there are usually alternatives of varying degrees of effectiveness. For problems that are not life-threatening, one option may be to do nothing. The next question to ask the doctor is “are there non-surgical or minimally-invasive therapies available to treat my condition?”
It is important to ask about your doctor’s experience doing any operation that has been proposed. You should feel comfortable with the number of procedures he or she has performed for problems like yours. For some of the newer procedures, such as endometrial ablation, laparoscopic surgery, or laparoscopic hysterectomy, additional training and experience must be acquired before the procedures can be safely performed. Regular, ongoing performance of these procedures is needed to keep surgical skills at a high level. Therefore, it is important for you to ask about surgical training and experience.
Should You Get a Second Opinion?
If surgery is recommended, often the answer is yes. Most doctors will welcome the idea of a second opinion. If they have done a complete job on the diagnosis and on the explanation of the problem to you, then they should feel confident about the range of options they have discussed with you. In addition, no doctor knows everything, and your doctor may welcome any other new ideas about your problem. This is your body and your life and you deserve to know everything you can about all the options available.
Laparoscopic Hysterectomy Compared to Abdominal Hysterectomy
A prospective, randomized, multi-centered study concluded that laparoscopic-assisted hysterectomy offered the benefits of less invasive surgery without increased risk. Estimated blood loss, postoperative day 1 hemoglobin, postoperative pain (as measured by a visual analog scale), and postoperative hospital stay were all significantly better for the laparoscopy-assisted hysterectomy group. The abdominal hysterectomy group had 7 postoperative complications; 1 woman with a cuff hematoma who required transfusion, 1 with delayed bleeding requiring reoperation and transfusion, and 5 other women with fevers. The only complications in the laparoscopic group were postoperative fevers in 2 women.
A retrospective cohort study compared laparoscopic hysterectomy in 34 women with uterine weights greater than 500 gms (range 500-1230 gms) to 68 women with uterine weights less than 300 gms. 101 The authors found no difference in complications rates, blood loss, hospital stay or postoperative recovery, but operating times were significantly shorter in the women with smaller uteri. No patient required conversion to laparotomy. Therefore, in experienced hands the benefits of laparoscopic hysterectomy may also be extended to women who have large myomas.
What are the Risks and Possible Complications of Hysterectomy
Major complications from a hysterectomy are rare. The risks include injury to the bladder, bowel, and ureters. While these injuries can be serious, if they are detected early they can usually be corrected. The Maine Women’s Study recently reported that only 1% of the 400 women in their study who had a hysterectomy had a bleeding complication, 5% had a treatable wound or bladder infection, and no woman had a serious complication or died. For all women in the United Sates ages 35 to 44 who have a hysterectomy (not for cancer) the risk of dying is about 3 per 10,000 women.
The largest study (about 4,000 surgeries) to measure complications from laparoscopic hysterectomy found that about 2% of women had a major complication, including one woman (0.002%) who died from a pulmonary embolus after surgery. Another study compared complications in 3112 laparoscopically assisted hysterectomies, 1618 abdominal hysterectomies. Injury to the bladder, ureter, and bowel was slightly more common with laparoscopic than abdominal procedures.
In studies of abdominal and vaginal hysterectomies, injury to the bladder has been reported in 1 out of 200 surgeries, and injury to the ureter in 1 out of 1,000 vaginal hysterectomies and in 1 out of 200 abdominal hysterectomies. In the Finnish study of laparoscopic hysterectomies, injury to the bladder was seen in 7 out of 1,000 surgeries, injury to the ureter in 1 out of 100, and injury to the intestine in 1 out of 250 women.
One study of women with fibroids reported 13% of women in the abdominal hysterectomy group had a complication including 1 bladder injury, 1 ureteral injury, 3 bowel injuries, 8 women who had nausea, vomiting and slow return of bowel movements, and 6 women with pelvic infections.
I have performed more than 500 laparoscopic hysterectomies and have never had an injury to the ureter or bowel or have a pelvic infection after surgery. Two women with multiple cesarean sections had a lot of scar tissue near their bladders from those surgeries and small holes made were made in the bladder. Laparoscopic suturing of these small injuries was done and the patients went home the next morning and had normal recoveries. In 29 years of an active gynecological surgery practice I have never had one patient die as a result of surgery.
(also see A Gynecologist’s Second Opinion (Plume, 2003) http://www.gynsecondopinion.com/hysterectomy.htm)
If you need a hysterectomy, should you also have your ovaries removed?
Women often have their healthy ovaries removed when they are having a hysterectomy (hysterectomy means removal of only the uterus) in order to prevent ovarian cancer from developing in the future. Data from the CDC show that 50% of women who have a hysterectomy between ages 40-44 have their ovaries removed, and 78% of women between ages 45-64 undergoing a hysterectomy have their ovaries removed. All together, about 300,000 American women have their healthy ovaries removed every year.
If the ovaries are removed before menopause, a sudden decrease in hormones made by the ovary, including estrogen, testosterone and androstenedione, results. We know that even after a woman enters menopause, her ovaries continue to make considerable amounts of testosterone and androstenedione, which are then changed into estrogen by other cells in the body.
Some studies show that women who keep their ovaries have a lower risk of heart disease. While ovarian cancer accounts for 14,700 deaths per year in the U.S., heart disease causes 326,900 deaths, and stroke causes 86,900 deaths each year. If a woman is not at high risk for ovarian cancer, then keeping the ovaries might benefit her overall health and survival. So, what is the best thing for a woman to do when faced with this issue?
The Study
Our study was designed to see whether it was better for women who needed a hysterectomy to keep their ovaries or have them removed during surgery. We used the database from the Nurses’ Health Study (NHS), which included 122,700 registered nurses in 1976 when it began. Over the past 24 years, 16,345 women had a hysterectomy and removal of their ovaries (oophorectomy), and 13,035 women had a hysterectomy with ovarian conservation (ovaries kept). We considered what diseases and conditions the women had, or died from, in the years after their surgery.
Results
The results showed that women who had their ovaries removed had a higher risk of death from any cause, and primarily from heart disease and lung cancer. Removing the ovaries at any age did not improve life-span for this group of women.
During the 24 years of follow-up, 34 of the 13,305 women (0.26%) who kept their ovaries died from ovarian cancer. While breast cancer and ovarian cancer were less frequent in women who had their ovaries removed, the overall risk of death from all types of cancer was higher among women who had their ovaries removed.
When we considered just the women who never used estrogen therapy after surgery, we found that women who had removal of their ovaries had a higher risk of stroke and lung cancer, and women who had removal of their ovaries before age 50 had a higher risk of heart disease, stroke and death from any cause.
Interpretation
For the past 35 years, doctors have recommended that women who needed a hysterectomy also consider having their ovaries removed in order to prevent the future development of ovarian cancer. Since ovarian cancer is difficult to detect and difficult to cure, most women having a hysterectomy chose to have their ovaries removed as well.
Our study questions the routine removal of women’s ovaries by showing that heart disease, stroke and lung cancer are more common in women who have their ovaries removed. And, since heart disease, stroke, and lung cancer are each much more common than ovarian cancer, many more women who have their ovaries removed will die of these conditions than can be saved from getting ovarian cancer.
As is true with all medical decisions, it is important to discuss these issues with your doctor. People often make very different decisions based on the same medical information. If you have a family history of heart disease or stroke, maybe keeping your ovaries makes more sense. Certainly, women with a strong family history of ovarian cancer, or women who know they have the genetic mutation (BRCA) that greatly increases their risk of ovarian and breast cancer, should strongly consider having their ovaries removed.
Scientific Abstract
Objective: To report long-term health outcomes and mortality following oophorectomy or ovarian conservation.
Methods: We conducted a prospective, observational study of 29,380 women participants of the Nurses’ Health Study who had a hysterectomy for benign disease; 16,345 (55.6%) had hysterectomy with bilateral oophorectomy and 13,035 (44.4%) had ovarian conservation. We evaluated incident events or death due to coronary heart disease, stroke, breast cancer, ovarian cancer, lung cancer, colorectal cancer, total cancers, hip fracture, pulmonary embolus, and death from all causes.
Results: Over 24 years of follow-up, for women with hysterectomy and bilateral oophorectomy, compared with ovarian conservation, the multivariable hazard ratios (HR) were 1.12 (95% CI 1.03, 1.21) for total mortality, 1.17 (95% CI 1.02, 1.35) for fatal plus nonfatal coronary heart disease (CHD), and 1.14 (95% CI 0.98, 1.33) for stroke. Although the risks of breast (HR 0.75 95% CI 0.68, 0.84), ovarian (HR 0.04 95% CI 0.01, 0.09), and total cancers (HR 0.92 95% CI 0.86, 0.98) decreased following oophorectomy, lung cancer incidence (HR =1.26, 95% CI 1.02, 1.56) and total cancer mortality (HR=1.17, 95% CI 1.04, 1.32) increased. For never-users of estrogen therapy, bilateral oophorectomy before age 50 was associated with an increased risk of all-cause mortality, CHD, and stroke. With an approximate 35-year life span after surgery, one additional death would be expected for every nine oophorectomies performed.
Conclusions: Compared with ovarian conservation, bilateral oophorectomy at the time of hysterectomy for benign disease is associated with a decreased risk of breast and ovarian cancer, but an increased risk of all-cause mortality, fatal and non-fatal coronary heart disease and lung cancer. In no analysis or age-group was oophorectomy associated with increased survival.
For more information about this important topic, please visit http://www.ovaryresearch.com/
Are There Reasons Some Women May Wish to Have Their Ovaries Removed?
However, there are a few situations where women may wish to have their ovaries removed at the time of hysterectomy. If the ovaries are affected by endometriosis or a woman has severe endometriosis and pelvic pain, studies show that removing the ovaries is associated with better long-term relief of pain than if the ovaries are not removed. Severe adhesions, or scar tissue, around the ovaries may also cause continued pelvic pain.
Some women have a family history of ovarian cancer. A genetic counselor can help evaluate your risk and may suggest BRCA (breast/ovarian cancer) gene testing to determine if you have inherited this gene that increases your risk. If you have an increased risk, you should strongly consider having your ovaries removed. In this case, the benefits of removing your ovaries and preventing ovarian cancer should far outweigh the benefits of keeping your own ovarian hormones.
Each woman needs to weigh the risks and benefits of having the ovaries removed at the time of surgery. Women tend to make very different decisions based on their particular circumstances. However, it is always best to make these decisions based on accurate and current medical information. This decision is yours to make and should be discussed in detail with your doctor. As always, if there are unanswered questions or concern, get a second opinion.
FOR MORE ABOUT HYSTERECTOMY, SEE OUR BOOK “A GYNECOLOGIST’S SECOND OPINION” AT http://www.gynsecondopinion.com/
William H. Parker, MD
Clinical Professor, Reproductive Medicine, UC San Diego School of Medicine
Page last updated: January, 2018